A National and International Crises
Suicide is often misunderstood and stigmatized like most mental health challenges. It must be noted that suicide continues to be one of the greatest challenges faced by mental health clinicians and researchers in recent times. The increasing trends in global suicide rates make an already complex situation even more difficult.
Suicide behavior disorder (SBD) was introduced in DSM-5 as a disorder for further consideration and potential acceptance into the diagnostic system. It only makes sense, in recognition of suicide’s importance as a psychiatric complication, the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders or DSM-5 has taken a major step in suggesting Suicidal Behavior Disorder (SBD) as a “condition for further study.”
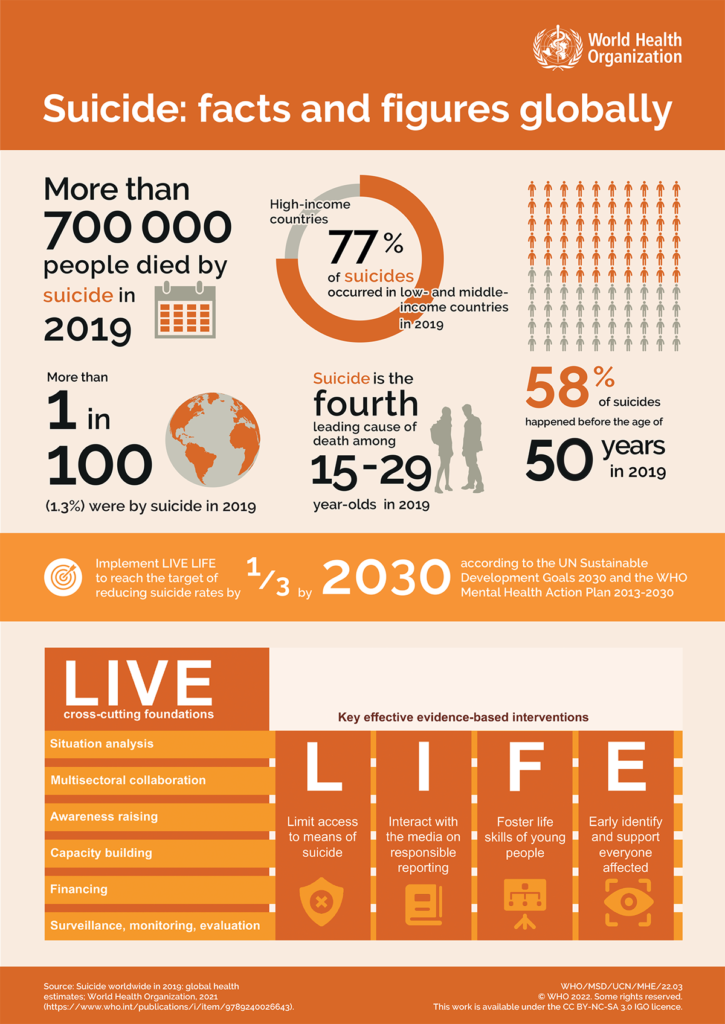
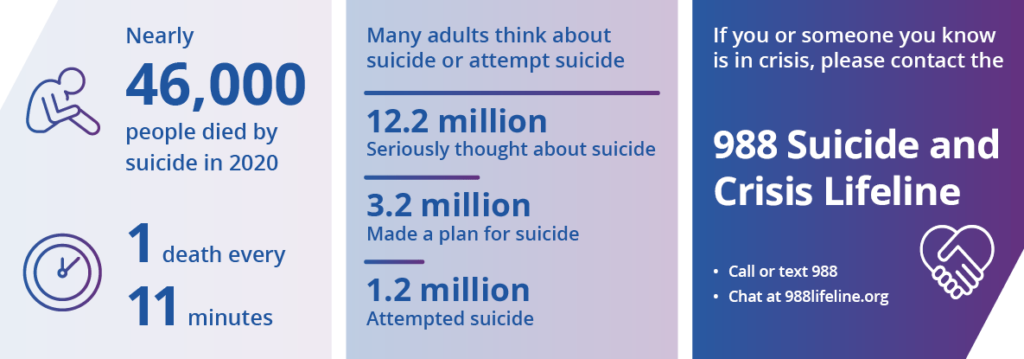
According to the National Institute of Mental Health (NIMH), suicide is a major public health concern and is currently the 12th leading cause of death overall in the United States. In 2020 alone, suicide claimed that lives of almost 46,000 people in the US alone. To put this into some perspective the average sports stadium’s capacity is 38,000. The World Health Organization (WHO) states the global number of deaths by suicide is more than 700,000 people each year.
What We Know Now, Planning for Action Now
What is suicide? Suicide is when people harm themselves with the goal of ending their life, and they die as a result. A suicide attempt is when people harm themselves with the goal of ending their life, but they do not die. The CDC estimated that in 2020, 12.2 million American adults seriously thought about suicide, 3.2 million planned a suicide attempt, and 1.2 million attempted suicides.
Every suicide is a tragedy which deeply affects families, communities and entire countries and has long-lasting effects on the people left behind. Suicide is complicated and tragic, but it is often preventable. Many factors contribute to suicide risk, however, knowing the warning signs for suicide and how to get help can help save lives.
Suicide is rarely caused by a single circumstance or event. Instead, a range of factors can increase the risk, including at the individual, relationship, community, and societal levels. The risk factors listed below are situations or problems which can increase the possibility that a person will attempt suicide:
Individual Risk Factors
- Previous suicide attempt
- History of depression and other mental illnesses
- Serious illness such as chronic pain
- Criminal/legal problems
- Job/financial problems or loss
- Impulsive or aggressive tendencies
- Substance misuse
- Current or prior history of adverse childhood experiences
- Sense of hopelessness
- Violence victimization and/or perpetration
Relationship Risk Factors
- Bullying
- Family/loved one’s history of suicide
- Loss of relationships
- High conflict or violent relationships
- Social isolation
Community Risk Factors
- Lack of access to healthcare
- Suicide cluster in the community
- Stress of acculturation
- Community violence
- Historical trauma
- Discrimination
Societal Risk Factors
- Stigma associated with help-seeking and mental illness
- Easy access to lethal means of suicide among people at risk
- Unsafe media portrayals of suicide
Complexity Requires Systemic-Focused Approach
As you finish reading this blog another person will have died from suicide. The question now becomes ‘What can we do?’ Most often the focus has been on prevention with regards to suicide. However, because of its complexity most prevention programs often fall short as the rates of occurrence continues to climb. Instead, the need becomes more focused on a systemic approach for increasing systems collaborations in support of overall well-being.
The phrase ‘Connection is protection’ has meaning on so many levels including individual, relationship, community, and societal. It is essential for human beings to have connections with others, where they are able to relate to someone or something allowing them to be comfortable sharing space. The Transformational Collaborative Outcomes Management or TCOM Tools are an outstanding examples of how systems (schools, community, health) can effectively collaborate, supporting our work of Connecting Through Communication-The Human Experience.

We have existing systems already attached to our lives, including family system (our family of origin or current family constellation), school/work (education, vocational) and primary health (primary care physician). The disconnect is often that these systems rarely, if ever, connect in any way. What if…a school-aged youth begins to have difficulty at school, withdrawing from friends and activities? Then that individual’s school reached out to the caregiver immediately upon noticing this change to let them know. Then they schedule an appointment with the family doctor who, during a wellness check-up, uncovers something.
This scenario was chosen specifically for the fact that the rate of teen suicides, ages 15-19 year, increased 56% over a decade in 2019. A recent report from the Centers for Disease Control and Prevention (CDC) shows that the teen suicide rate in the United States has skyrocketed in recent years. Suicide was recently ranked as the second-leading cause of death for people between the ages of 15 and 24 years old.
TRANSFORM CARE INTO VALUE
Improve Outcomes and Care Efficiency
Opeeka’s Person-Centered Intelligence Solution (P-CIS) connects to existing electronic health records and automates processes to improve care delivery.
Improving Well-Being by Identifying What Works
Well-being is as challenging to define as it is to develop a clear plan for achieving it. We, at Opeeka, know that almost every person struggles with well-being from time to time, and for some it is a lifelong battle. Opeeka’s mission is to promote well-being for all, especially for those who benefit from occasional reminders of gratitude for those struggling with depression, addiction, homelessness, safety, and/or physical challenges. If we can conceptualize well-being as a ladder, then our goal is to help empower every person to take upward steps.
Opeeka offers a suite of behavioral health efficiency solutions for data collection, care planning, activity tracking, alert generation, outcomes monitoring, warehousing, and analytics tools through our Person-Centered Intelligence Solutions or P-CIS (pronounced pieces). Our customers range from state departments that manage healthcare, behavioral health or child welfare to private healthcare payers and providers, community-based providers, and individual providers.
Let’s collaborate to coordinate compassionate care TODAY! Contact us at www.opeeka.com or (866) OPEEKA1 (673-3521) to see how our P-CIS tracks well-being over time (in real-time) to identify the true impact of care. Everyone’s circumstances are unique and what may be helpful to one person may be less so for another. That is why Whole Person-Centered Care is so important!
FAQs
Suicide is when a person harms themselves with the intention of ending their life, leading to death. Suicide behavior disorder (SBD) is a disorder introduced in DSM-5 as a condition for further consideration and potential acceptance into the diagnostic system.
According to the National Institute of Mental Health (NIMH), suicide is currently the 12th leading cause of death overall in the United States, claiming almost 46,000 lives in 2020 alone. The World Health Organization (WHO) states the global number of deaths by suicide is more than 700,000 people each year.
There are several risk factors that can increase the possibility that a person will attempt suicide. These include individual risk factors such as previous suicide attempts, history of depression and other mental illnesses, substance misuse, and violence victimization and/or perpetration. Relationship risk factors include bullying, family/loved one’s history of suicide, and high conflict or violent relationships. Community risk factors include lack of access to healthcare, suicide cluster in the community, and community violence. Societal risk factors include stigma associated with help-seeking and mental illness, easy access to lethal means of suicide among people at risk, and unsafe media portrayals of suicide.
While prevention programs are often focused on preventing suicide, the complexity of the issue requires a systemic approach for increasing systems collaborations in support of overall well-being. Collaboration and connection on individual, relationship, community, and societal levels are essential. The Transformational Collaborative Outcomes Management (TCOM) Tools are an example of how systems can effectively collaborate and support overall well-being.
Opeeka’s mission is to promote well-being for all, especially for those who benefit from occasional reminders of gratitude for those struggling with depression, addiction, homelessness, safety, and/or physical challenges.
Conclusion
In conclusion, suicide remains a major public health concern both nationally and globally. The increasing trends in global suicide rates highlight the need for a systemic approach to suicide prevention. While there are individual, relationship, community, and societal risk factors for suicide, knowing the warning signs and how to get help can help save lives. Collaboration between existing systems such as family, school, and primary health care is vital for early identification and prevention of suicide. It is important to prioritize well-being and promote connections to help prevent suicide. As a society, we must continue to work towards breaking down the stigma surrounding mental health challenges, including suicide, and take action towards preventing this tragic loss of life.